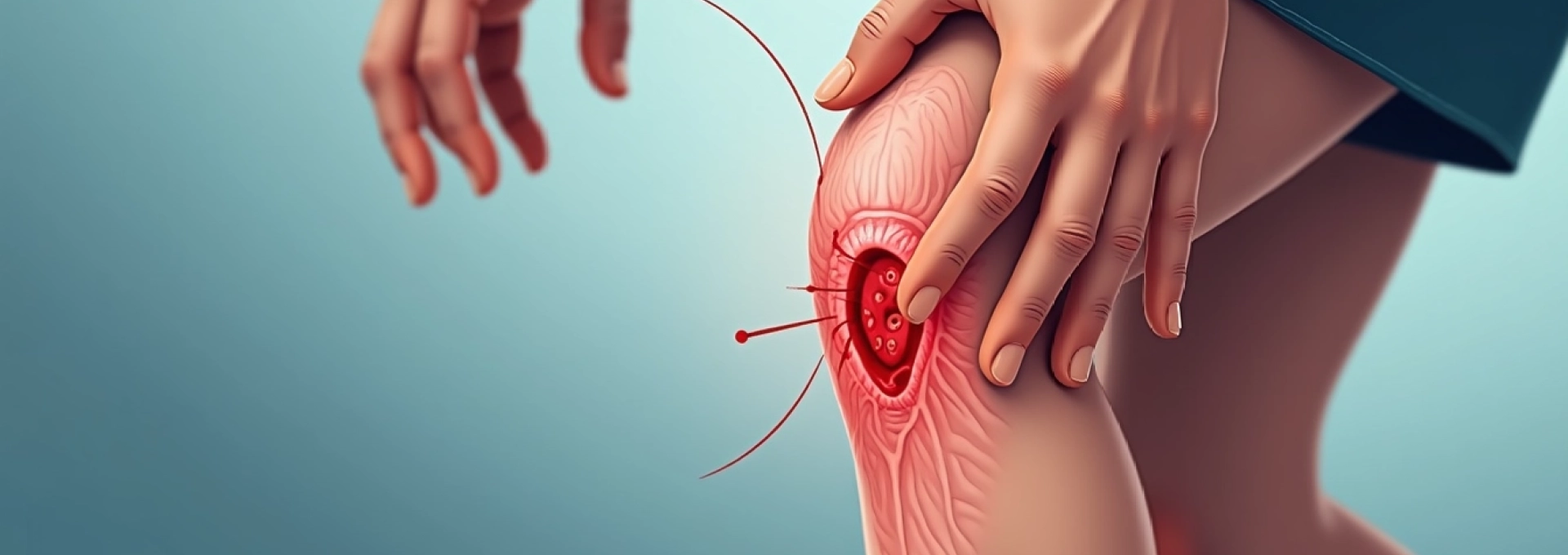
Knee wounds are among the most common injuries encountered in both clinical and domestic settings, yet they present unique challenges when it comes to infection management. The knee’s complex anatomy, constant movement, and exposure to environmental contaminants create an ideal environment for bacterial proliferation. When a simple cut transforms into an infected wound, prompt recognition and appropriate intervention become crucial for preventing serious complications such as cellulitis, osteomyelitis, or systemic sepsis. Understanding the clinical indicators of infection, implementing proper wound care protocols, and knowing when to seek professional medical intervention can mean the difference between a straightforward recovery and a prolonged, complicated healing process.
Clinical recognition of knee wound infection signs
Recognising the early signs of wound infection requires a systematic approach to clinical assessment. Wound infection typically manifests within 24 to 72 hours following the initial injury , though some infections may develop more gradually over several days. The key to successful management lies in distinguishing between normal inflammatory responses and pathological infection markers. Healthcare professionals and patients alike must understand that not all redness or swelling indicates infection, as these can be part of the body’s natural healing process.
Erythema and cellulitis progression patterns
The progression of erythema in infected knee wounds follows predictable patterns that can guide clinical decision-making. Initial redness around a wound is typically confined to the immediate injury site and measures less than 2 centimetres in diameter. However, when infection develops, this erythema begins to spread in a characteristic pattern, often extending beyond the original wound margins in irregular, finger-like projections. The affected skin becomes warm to touch and may develop a glossy appearance as the infection progresses.
Cellulitis, a deeper soft tissue infection, presents with more extensive erythema that spreads rapidly along fascial planes. The infected tissue becomes indurated and painful, with clearly demarcated borders that advance over hours rather than days. Red streaking extending proximally from the wound site indicates lymphangitis, a serious complication requiring immediate medical attention. This streaking pattern typically follows the natural lymphatic drainage pathways and may be accompanied by palpable lymphadenopathy in the regional nodes.
Purulent discharge and exudate assessment
The character and quantity of wound exudate provide valuable diagnostic information about infection status. Normal healing wounds produce minimal, clear to slightly yellow serous fluid that decreases over time. In contrast, infected wounds typically produce purulent discharge characterised by its thick, opaque consistency and characteristic odour. The colour of purulent material can vary significantly depending on the causative organism, ranging from yellow-green associated with Pseudomonas infections to thick, creamy white discharge typical of Staphylococcal infections.
Assessment of exudate volume is equally important, as infected wounds often produce disproportionately large amounts of discharge compared to their size. The presence of frank pus or cloudy fluid draining from the wound represents a clear indication of bacterial colonisation. Additionally, the formation of yellow crusting around wound edges or the development of satellite pustules in the surrounding skin suggests spreading infection that requires aggressive management.
Systemic infection symptoms: fever and lymphadenopathy
Systemic manifestations of wound infection indicate that the body’s local immune response has been overwhelmed, potentially leading to bacteraemia or sepsis. Fever, defined as a core body temperature exceeding 38°C (100.4°F), represents one of the most significant warning signs of systemic involvement. However, it’s important to note that elderly patients or those with compromised immune systems may not develop fever despite serious infections , making other clinical indicators even more crucial for diagnosis.
Regional lymphadenopathy develops as lymph nodes work to filter bacteria and inflammatory mediators from the infected tissue. In knee wound infections, the inguinal and popliteal lymph nodes are most commonly affected, becoming enlarged, tender, and sometimes fluctuant if abscess formation occurs. The presence of lymphangitis, visible as red streaking extending from the wound toward these regional nodes, indicates active bacterial spread through the lymphatic system and requires immediate medical intervention.
Pain escalation and functional mobility impairment
Pain assessment in infected knee wounds requires careful consideration of both intensity and character. While initial wound pain typically follows a predictable pattern of gradual improvement over the first 48-72 hours, infected wounds demonstrate escalating pain that worsens rather than improves with time . This pain often has a throbbing, pulsatile quality and may be accompanied by significant tenderness that extends well beyond the original wound boundaries.
Functional assessment reveals progressive mobility impairment as infection advances. Patients typically report increasing difficulty with weight-bearing, knee flexion, and normal ambulation. The combination of pain, swelling, and inflammatory response can lead to protective muscle spasms that further limit range of motion. When infection progresses to involve deeper structures, patients may experience severe functional limitations that persist even with adequate pain management, indicating the need for more aggressive intervention.
Immediate wound care protocol for infected knee lacerations
Effective management of infected knee wounds requires a systematic approach that combines thorough wound assessment with appropriate interventional strategies. The primary goals include controlling bacterial proliferation, optimising wound healing conditions, and preventing progression to deeper tissue involvement. Time-sensitive intervention within the first 24-48 hours of recognising infection signs significantly improves treatment outcomes and reduces the likelihood of complications. Healthcare providers must balance aggressive treatment with preservation of healthy tissue to achieve optimal functional and cosmetic results.
Sterile irrigation with normal saline solution
Mechanical irrigation represents the cornerstone of infected wound management, effectively removing debris, bacteria, and inflammatory mediators from the wound bed. Normal saline solution, delivered at appropriate pressure (8-15 psi), provides optimal cleaning without causing additional tissue damage. The irrigation process should begin with gentle flushing using a large-volume syringe or irrigation system, progressively increasing pressure as tolerated to dislodge adherent material.
The volume of irrigation fluid should be substantial, typically requiring 50-100ml per centimetre of wound length for adequate cleaning. Pulsatile irrigation systems offer superior cleaning effectiveness compared to simple flushing, particularly for wounds with complex geometry or significant contamination. Following initial irrigation, the wound should be carefully inspected for retained foreign material, devitalised tissue, or signs of deeper infection that may require surgical intervention.
Antiseptic cleansing using chlorhexidine or Povidone-Iodine
Antiseptic agents play a crucial role in reducing bacterial load and preventing further colonisation of infected wounds. Chlorhexidine gluconate, available in concentrations ranging from 0.05% to 4%, demonstrates broad-spectrum antimicrobial activity with residual effects lasting several hours post-application. For infected knee wounds, a 0.05% chlorhexidine solution provides effective bacterial reduction while minimising cytotoxicity to healing tissues.
Povidone-iodine represents an alternative antiseptic option, particularly effective against gram-positive organisms commonly associated with skin and soft tissue infections. However, its use requires careful consideration of potential adverse effects, including tissue irritation and interference with wound healing when used in high concentrations or for extended periods. Diluted povidone-iodine solutions (0.001-0.01%) maintain antimicrobial efficacy while reducing tissue toxicity , making them suitable for infected wound management.
Debridement techniques for necrotic tissue removal
Surgical debridement of necrotic or infected tissue is often necessary to establish a clean wound bed conducive to healing. Sharp debridement, performed with sterile instruments, allows precise removal of devitalised tissue while preserving viable structures. This technique requires careful assessment of tissue viability, with healthy tissue typically appearing pink or red with good bleeding response, while infected or necrotic tissue appears grey, black, or has a stringy, adherent quality.
Conservative debridement approaches, including enzymatic or autolytic methods, may be appropriate for patients who cannot tolerate surgical intervention or when the extent of tissue involvement is limited. Enzymatic debriding agents, such as collagenase-based preparations, selectively target necrotic tissue while sparing healthy structures. Autolytic debridement utilises the body’s natural enzymes to break down devitalised tissue, though this process requires adequate wound moisture and may be too slow for actively infected wounds.
Appropriate dressing selection and application methods
Dressing selection for infected knee wounds must balance infection control with optimal healing conditions. Antimicrobial dressings containing silver, iodine, or honey provide sustained antibacterial activity while maintaining appropriate wound moisture levels. Silver-impregnated dressings offer broad-spectrum antimicrobial coverage with minimal risk of resistance development, making them particularly suitable for infected wounds with mixed bacterial populations.
The application technique significantly influences dressing effectiveness and patient comfort. Infected wounds require frequent dressing changes, typically every 24-48 hours, depending on exudate levels and clinical response. Proper securing techniques that accommodate knee movement while maintaining dressing integrity present unique challenges, often requiring specialised tape or securing systems designed for high-mobility areas. The dressing should extend adequate distances beyond the wound margins to prevent contamination while allowing for normal range of motion.
Antibiotic treatment strategies for knee wound infections
Antibiotic selection for infected knee wounds requires consideration of multiple factors, including the severity of infection, likely causative organisms, patient allergies, and local resistance patterns. Empirical antibiotic therapy should target the most common pathogens while awaiting culture and sensitivity results, which can take 48-72 hours to complete. Staphylococcus aureus, including methicillin-resistant strains (MRSA), and Streptococcus pyogenes represent the most frequent isolates from skin and soft tissue infections, though gram-negative organisms may be involved in certain circumstances.
Mild to moderate infections without systemic involvement often respond to oral antibiotic therapy. First-line agents include cephalexin, clindamycin, or trimethoprim-sulfamethoxazole, depending on local resistance patterns and patient factors. Cephalexin provides excellent coverage against most staphylococcal and streptococcal species, with good tissue penetration and a favourable side effect profile. Clindamycin offers the additional benefit of anti-toxin effects, particularly valuable in suspected streptococcal infections where toxin production contributes to tissue damage.
Severe infections or those with systemic manifestations require parenteral antibiotic therapy, often necessitating hospitalisation for close monitoring and intravenous access. Vancomycin remains the gold standard for suspected or confirmed MRSA infections, though newer agents such as linezolid, daptomycin, or ceftaroline may offer advantages in specific situations. Combination therapy may be necessary for polymicrobial infections or when gram-negative coverage is required, particularly in wounds with significant contamination or in immunocompromised patients.
The duration of antibiotic therapy typically ranges from 7-14 days, depending on clinical response and infection severity, with longer courses reserved for complicated infections involving deeper structures or those with delayed clinical improvement.
Monitoring treatment response involves regular assessment of clinical parameters, including wound appearance, surrounding erythema, systemic symptoms, and functional improvement. Failure to demonstrate clinical improvement within 48-72 hours of initiating appropriate therapy suggests the need for treatment modification, which may include antibiotic adjustment based on culture results, surgical intervention, or investigation for underlying complications such as osteomyelitis or retained foreign material.
Professional medical intervention and emergency indicators
Certain clinical presentations mandate immediate professional medical evaluation and potential emergency intervention. Red streaking extending from the wound site toward the torso indicates lymphangitis and potential progression to systemic infection, requiring urgent antibiotic therapy and close monitoring. Similarly, the development of fever, chills, or other systemic symptoms in the context of a wound infection suggests bacteraemia and the need for immediate medical attention, including blood cultures and parenteral antibiotic administration.
Deep infections involving fascial planes or underlying bone present particularly serious complications that require surgical consultation. Signs suggesting deep involvement include severe pain disproportionate to the apparent wound severity, woody induration of surrounding tissues, or clinical signs of compartment syndrome such as increased pain with passive movement. Crepitus or gas formation within the wound may indicate necrotising fasciitis or gas gangrene, life-threatening conditions requiring emergency surgical debridement and aggressive antibiotic therapy.
Patients with diabetes, peripheral vascular disease, or immunosuppression face significantly higher risks of severe complications from wound infections and typically require lower thresholds for professional intervention. These individuals may not mount typical inflammatory responses to infection, making clinical recognition more challenging while simultaneously increasing the risk of rapid progression to serious complications. Regular wound assessment by healthcare professionals, rather than self-monitoring alone, becomes essential for these high-risk populations.
Emergency department evaluation should be sought immediately if signs of sepsis develop, including altered mental status, rapid heart rate, low blood pressure, or difficulty breathing in the context of a wound infection.
Surgical intervention may be necessary for infected wounds that fail to respond to conservative management or those with evidence of deep tissue involvement. Procedures can range from simple incision and drainage of localised abscesses to extensive debridement of necrotic tissue or fasciotomy for compartment syndrome. The timing of surgical intervention significantly influences outcomes, with early aggressive treatment typically yielding better results than delayed intervention after complications have developed.
Complications prevention and long-term wound management
Preventing complications in infected knee wounds requires a comprehensive approach addressing both immediate infection control and factors that may impede healing. Patient education regarding proper wound care techniques and recognition of warning signs plays a crucial role in preventing progression to serious complications. Patients must understand the importance of maintaining wound cleanliness, adhering to prescribed antibiotic regimens, and seeking prompt medical attention for any concerning changes in wound appearance or symptoms.
Chronic wound development represents a significant long-term complication that can result from inadequately treated acute infections. Factors contributing to chronicity include persistent bacterial colonisation, repeated trauma to the healing tissue, underlying medical conditions affecting wound healing, and inappropriate wound care techniques. Biofilm formation within chronic wounds creates particular challenges, as bacteria embedded within protective extracellular matrices demonstrate increased resistance to both antimicrobial agents and host immune responses.
Nutritional optimisation plays an often-overlooked role in wound healing and infection prevention. Adequate protein intake, essential for collagen synthesis and immune function, becomes particularly important during the healing phase. Vitamin C deficiency can significantly impair wound healing, while zinc deficiency affects both immune function and tissue repair processes. Patients with infected wounds should receive nutritional counselling to ensure adequate intake of these essential nutrients, with supplementation considered when dietary intake appears insufficient.
Long-term follow-up protocols should include regular wound assessment, monitoring for signs of recurrent infection, and evaluation of functional outcomes. Scar tissue formation and joint stiffness represent common sequelae of infected knee wounds, potentially requiring physical therapy intervention to restore normal range of motion and function. Early mobilisation, when clinically appropriate, helps prevent joint contractures and promotes optimal functional recovery while maintaining wound healing progress.
| Complication | Risk Factors | Prevention Strategies | Treatment Approach |
|---|---|---|---|
| Cellulitis | Delayed treatment, immunocompromise | Early antibiotic therapy, proper wound care | Parenteral antibiotics, surgical debridement if needed |
| Osteomyelitis | Deep wounds, diabetes, vascular disease | Thorough wound cleaning, adequate antibiotic course | Prolonged antibiotic therapy, surgical intervention |
| Sepsis | Systemic illness, multiple comorbidities | Prompt recognition, early aggressive treatment | ICU management, broad-spectrum antibiotics |
The psychological impact of infected wounds, particularly those resulting in visible scarring or functional limitation, should not be underestimated. Patients may experience anxiety about wound appearance, fear of recurrent infection, or depression related to activity limitations during the healing process. Counselling and support services can play valuable roles in comprehensive wound management, helping patients cope with both the physical and emotional aspects of recovery. Healthcare providers should maintain awareness of these
psychological challenges may require additional support resources and referral to appropriate mental health professionals when indicated.
Regular wound surveillance protocols should be established for patients with healed infected wounds, particularly those at high risk for recurrence. This includes patients with diabetes, peripheral vascular disease, or occupational exposures that increase wound risk. Monthly self-examinations of previously infected sites can help identify early signs of tissue breakdown or recurrent infection, enabling prompt intervention before serious complications develop. Healthcare providers should provide detailed instructions on self-examination techniques and clear guidelines for when to seek professional evaluation.
The development of antibiotic-resistant organisms represents an increasingly important consideration in wound infection management. Inappropriate antibiotic use, including inadequate duration of therapy or inappropriate spectrum coverage, can contribute to resistance development and subsequent treatment failures. Antimicrobial stewardship principles should guide all antibiotic prescribing decisions, with culture-directed therapy preferred over prolonged empirical treatment whenever possible. This approach not only optimises individual patient outcomes but also helps preserve antibiotic effectiveness for future patients.
Long-term complications from infected knee wounds can include chronic osteomyelitis, recurrent cellulitis, lymphedema, and permanent functional impairment, making prevention and early aggressive treatment essential for optimal outcomes.
Wound healing optimisation extends beyond infection treatment to include modification of risk factors that may impair tissue repair. Smoking cessation represents one of the most important interventions, as nicotine causes vasoconstriction that significantly impairs wound healing and increases infection risk. Similarly, optimal glycemic control in diabetic patients, blood pressure management in hypertensive individuals, and nutritional optimisation all contribute to improved healing outcomes and reduced complication rates. Collaborative care involving multiple healthcare disciplines often provides the most comprehensive approach to addressing these multifactorial influences on wound healing.
The integration of advanced wound care technologies, including negative pressure wound therapy, bioengineered skin substitutes, and growth factor applications, may be beneficial for complex or chronic infected wounds that fail to respond to conventional treatment. These interventions should be considered as adjuncts to, rather than replacements for, proper wound care fundamentals and appropriate antimicrobial therapy. The decision to implement advanced therapies requires careful cost-benefit analysis and consideration of patient-specific factors that may influence treatment success.